At midnight, an EMS crew responds to a 911 call for chest pain.
The patient is a 40 yo male who developed chest pain while lifting weights 45 minutes ago. His wife called 911 when he was having trouble sleeping secondary to the pain. He appears diaphoretic and unwell.
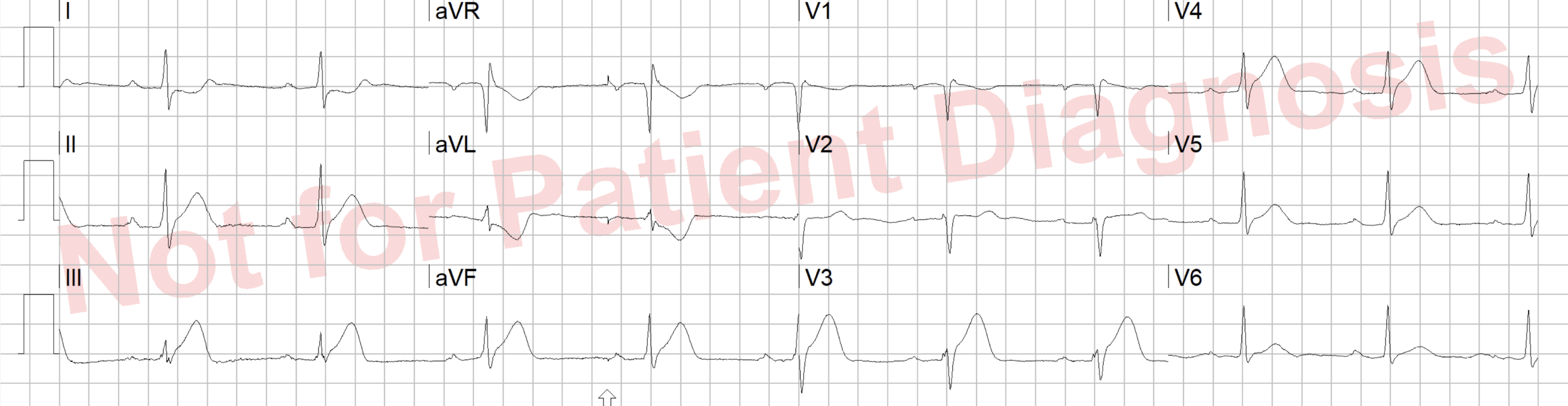
EMS obtains the following ECG :
They administer aspirin and begin transport to the hospital. The paramedic is concerned for an acute myocardial infarction as the patient appear unwell, and they recognize hyperacute inferior T waves and ST depression and T wave inversion in aVL.
Should they bypass the closest hospital to transport to the PCI center? Should they activate an MI alert prior to hospital arrival?
In 2018, the Emergency Medicine community was introduced to the concept of Occlusion Myocardial Infarction when Meyers, Weingart and Smith self-published the OMI Manifesto.
The big idea? ST elevation on the ECG is an unreliable tool for detecting patients in whom emergent reperfusion therapy is indicated – namely, those with an acute occlusion of a coronary artery.
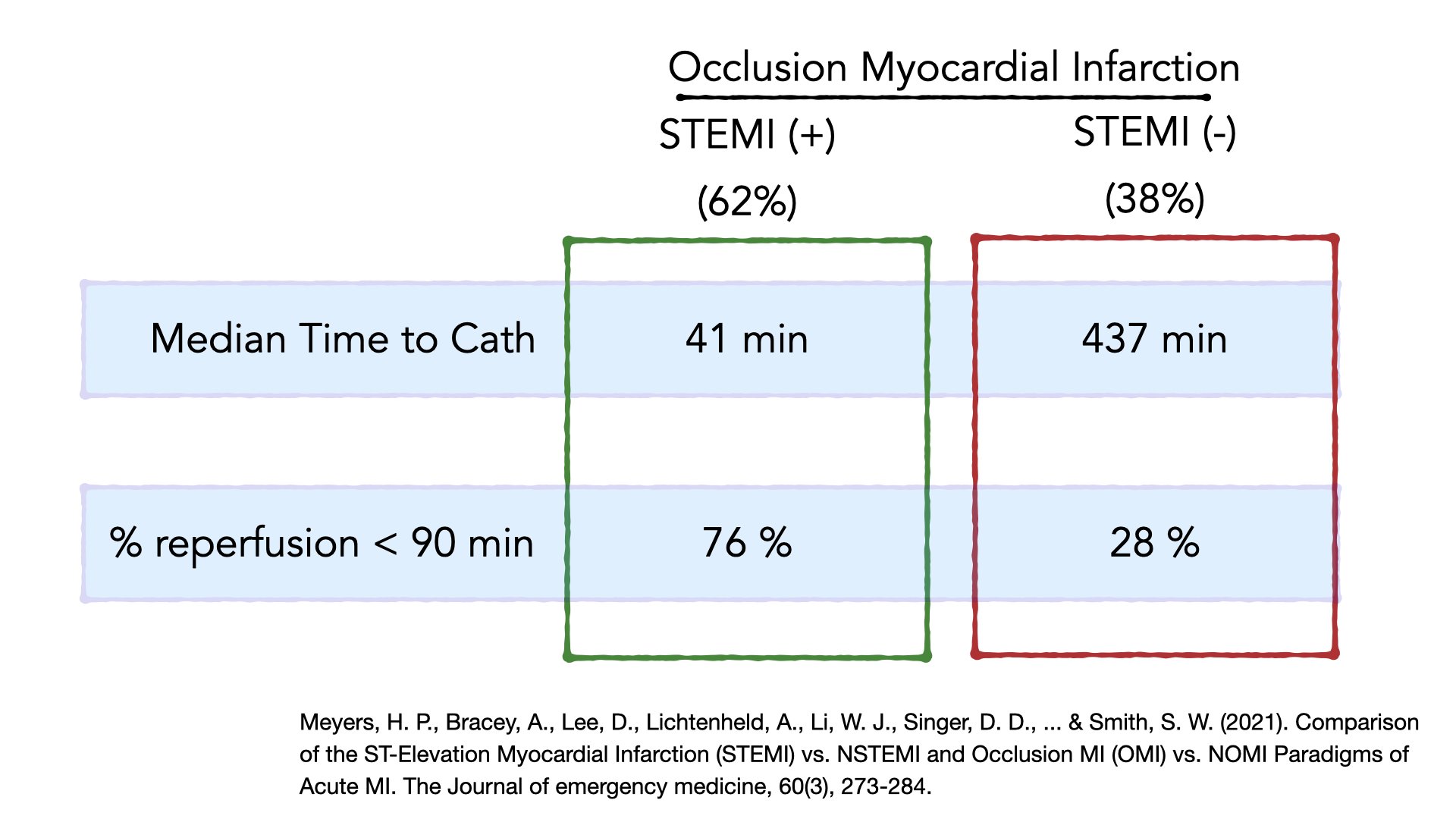
Subsequently, Myers et. al. published a retrospective chart review which lent some evidence to the ideas put forth in the OMI manifesto: 38% of patients with an acute occlusion of a coronary artery did not meet STEMI criteria. The result? A significant delay to reperfusion therapy.
Given these results, should EMS begin to shift a focus from “STEMI systems of care” to “OMI systems of care”? Why or why not?
Please share your thoughts and commentary below by December 20th to be included in the summary post.