In February, we posted the following Discussion Forum stem:
EMS is dispatched to a cardiac arrest at a residence with bystander CPR in progress.
The paramedic and EMT partners arrive on scene to find BLS care being initiated by a company of four firefighters who are credentialed at either the EMR or EMT level.
The paramedic focuses on coordinating the resuscitation including ensuring the priorities of early defibrillation and high-quality CPR, as well as accomplishing the ALS tasks of obtaining IV/IO access and medication administration. While focusing on these priorities, the paramedic would like to off-load airway management to another on-scene provider so a supraglottic airway can be placed.
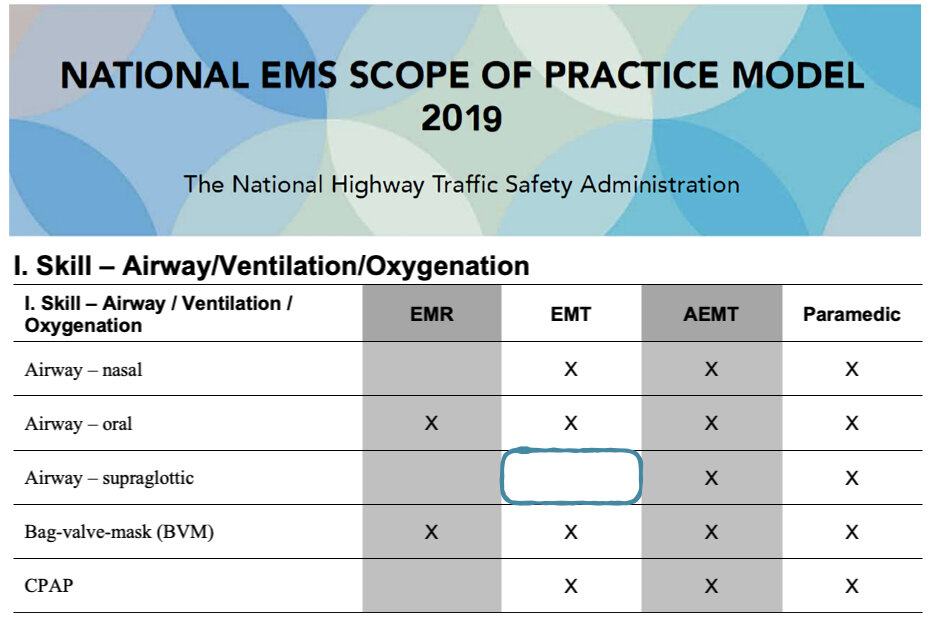
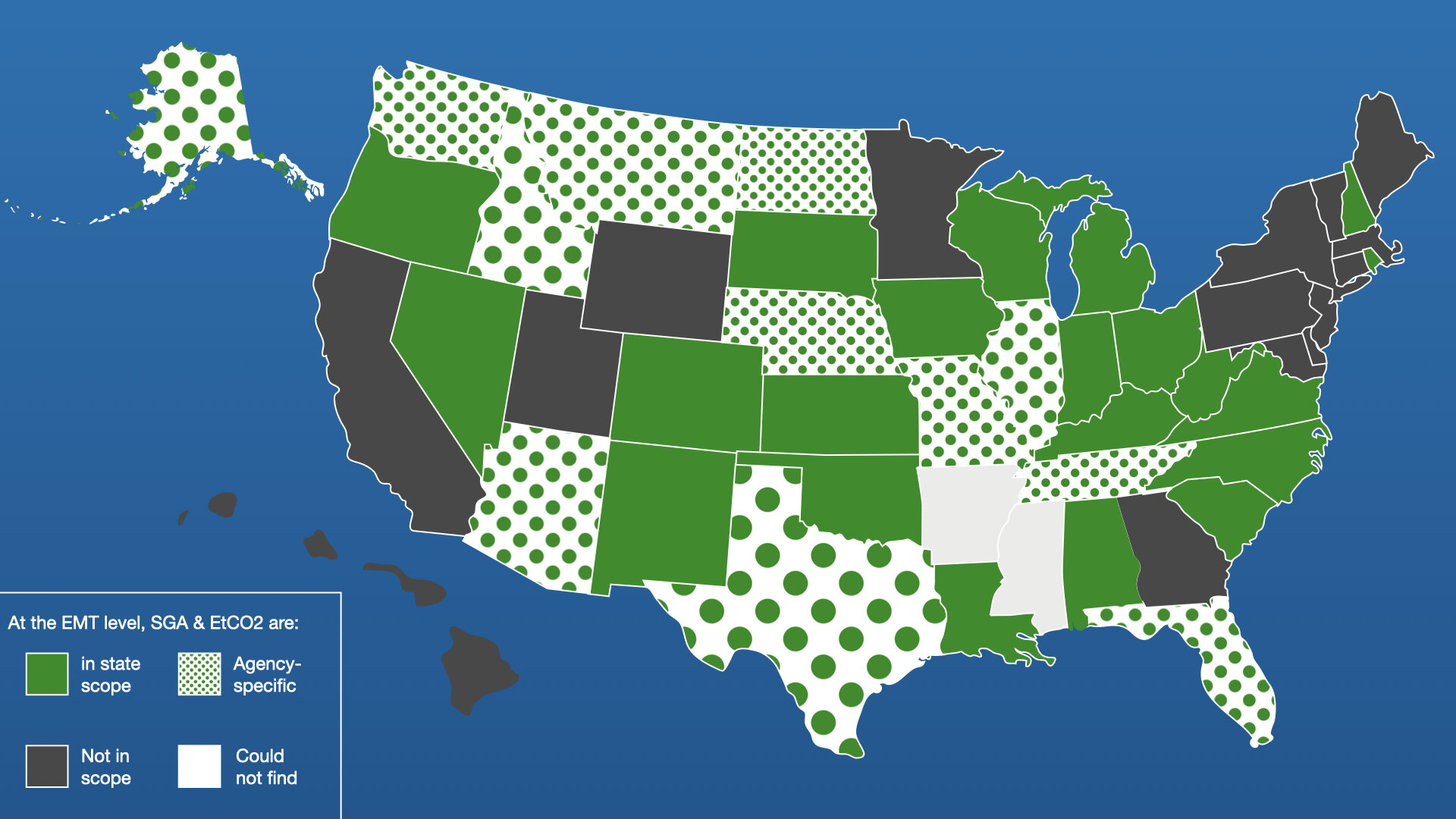
Supraglottic airway placement is not currently in the 2019 National Scope of Practice Model at the EMT level. However, some states, or where permissible EMS agencies, have placed this within the EMT scope. Based on survey data collected via the Discussion Forum post, and when possible, confirmed on the state website, the current map of supraglottic airway at the EMT scope of practice is below:
Figure 1: Scope of practice information collected by Discussion forum survey and confirmed by review of the state website when possible. Image credit: Maia Dorsett
There was substantial discussion regarding whether supraglottic airways should be at the EMT scope of practice. This discussion focused predominantly on three themes: (1) Advantages and ease of the skill, (2) need for capnography for airway confirmation and (3) the need for additional education and training commensurate with the complexity of not just the skill, but its indications and monitoring.
Advantages and Ease of skill
A number of comments addressed the relative ease of supraglottic airway placement as a psychomotor skill. Review of the evidence suggests that supraglottic airways – including laryngeal tubes and LMAs such as the iGel – have high first pass success rates, even in the hands of novices. Studies that focus specifically on SGA placement by BLS providers specifically confirm first pass success rates of > 80% and overall success rates of > 90% for the King-LT.[1,2]. One argument is that, at least in cardiac arrest, where SGA as a primary method of airway management has become more common, offloading this skill to EMTs allows ALS providers to focus on the overall the resuscitation. In addition, in rural areas with limited access to ALS providers, this gives BLS providers another airway management tool.
In South Carolina, SGA insertion is an EMT level skill. For my service and many others in the state that utilize a tiered response model it is used regularly by crews at the EMT level. The requirement for SGA placement is to have a device capable of monitoring capnography/capometry immediately available following device placement. For my service we do not utilize intubation as a first line airway device in cardiac arrest and since the practice was implemented 12 years ago along with some other changes we have seen a drastic increase in return of spontaneous circulation among cardiac arrest patients encountered. There is no reason SGA placement should not be an EMT level skill. – Austin Pace
EMTs are extremely capable of placing supraglottic airways. We have EMT level fire departments who often place these airways early on in the setting of cardiac arrest. With excellent training our EMTs have high success rates. Paramedics are not as plentiful in North Carolina and there are even fewer advanced EMTs in our State. We are teaching supraglottic airways in our initial EMT programs and we feel strongly that this should be part of the National Scope of practice for EMTs - Kim Woodward
With our paramedics doing so much else EMTs need to be able to fully manage airway. – Andie
“I believe …this would be allowed everywhere. They are easy to use and offer a way to secure the airway and get oxygen to the patient. I work in Michigan where this is allowed at the EMR level with IGels and colormetric.”- George F
Agree, we just added this to their skills with extra training. Especially in Idaho, my agency is very rural and only 2 man crew (1 paramedic and 1EMTB) rare fire back up. We have seen improved codes because of this.- Eric S Donahue
SGA and EtCO2 are both within the EMT scope of practice in both my current state of practice (New Hampshire) and my previous (Michigan). EtCO2 hasn't been available on most BLS rigs in my experience (except colorimetric detectors, I guess, which don't offer a lot but better than nothing), but it's something I was trained on by my service and used on ALS shifts. I absolutely used both King airways and i-gels as an EMT-B, and it's something I consider to be crucial for good patient care in the emergent setting. EMTs need to be able to manage airway without a babysitter, and if anything need more training on EtCO2 in the classroom setting. - Charlotte P
I allow in my services and we have incredibly high success rates with our supraglottic (we use igel, no financial relationship) device. Over 90% first pass success with EMT placement almost exclusively in cardiac arrest and 1/2 of our prehospital cardiac arrest airways are secured by EMT versus paramedic. we run around 400 cardiac arrests/year. - Ryan Jacobsen
Use of SGA is a permitted process in WA State. Our current data, using igel, is 80% success by BLS.- Marvin Wayne
I think that this is a "trainable" and valuable skill for EMT-B's, and the scope of practice should reflect this. - Ray Fowler
Both of these skills should be available to EMTs. We allow them to use a ventilator (BVM) but not isolate the pulmonary system thereby risking gastric insufflation and aspiration. Allowing the EMT to place a supraglottic device will also allow them to place a gastric decompression tube to improve ventilation. - Jeffrey Siegler
In Ohio, the placement of a supraglottic airway is strictly limited to pulseless and apneic patients at the EMT level. If a patient has a pulse, even if apneic, ventilation must be performed by another method, e.g. bag-valve-mask (BVM). For patients with a pulse, even if apneic, there is an increased risk of vomiting and/or aspiration if a supraglottic airway device is in place, compared to a BVM, due to the potential for the return of a gag reflex if the patient responds to assisted ventilation measures. - Carol Cunningham
Yes, This is just as simple as an OPA. - David S. Kugler
After three years of work, the State of Alaska is currently implementing its revised Scope of Practice. This includes SGA for EMT I (Basic) with Medical Director Sponsorship Required. Standing orders are required. Active involvement of the Medical Director in training is crucial. Our EMT II level (similar to Intermediate elsewhere) includes etCO2 monitoring and interpretation and IO, TXA, IV Dextrose. We have found that we can successfully teach etCO2 at the EMT II level. After removing ET intubation from this scope (SGA was already there), we found the time in the training to teach these other life-saving skills noted above. This is super important since AEMT and paramedic response are rare outside our larger cities. So EMT I or II is all you get in most communities. Dr. Levy and I agree that these skills can help to treat what can kill you now - Tom Quigley Peterson, Co-Chair, SOA Scope of Practice Committee
EMTs have always and should always be the masters of basic airway management to include OPA, NPA, BVM ventilation, and now that we have iGel LMAs which are quite easy to train providers to place, should absolutely be within the scope of practice of EMTs. This is especially important in the cardiac / respiratory arrest patient which then allows ALS personnel to focus on ALS interventions. iGels are easier to train EMTs to place than teaching hand ventilation with a BVM – Cstephens
Dr. Stephens ends with the discussion that iGels are easier to train than ventilation with a BVM. Indeed, a number of comments discussed specifically that BVM is actually a difficult - though very important – skill to perform well.
The difficulty of manual ventilation using a BVM is well documented in the literature. The difficulties are threefold;
-Inability to maintain a mask seal
-Inability to control volume
-Inability to control rate
Yet the BVM is a basic or foundational skill for all prehospital levels. Today, supraglottic airways such as the I Gel are simple in sizing, easy to place and help minimize the problem of mask seal. It would seem to me the scope of practice should be amended to add them to the EMT level. It would allow for better focus of volume and rate and hopefully better ventilation. - Jon Politis
“Less of a practice dependent skill than good BVM management. Allows adequate oxygenation and ventilation.”- Mike Carter
BVM ventilation are performed poorly at best from EMR through RT, MD. Without a strong push to bring providers up to "expert" level in there BLS skills SGA's have a place and a need. Without optimally clearing airway on initial contact, properly placing airway adjuncts, properly positioning patient for optimum patency of the airway, proper BVM seal and good ventilation techniques to prevent aspiration, gastric insufflation, barotrauma, or volutrauma. The use of SGA's can increase the margin of error in the above to allow more effective ventilation of the patient and provide some protection of the adverse effects of improper bagging techniques. So yes, I strongly urge WI to continue to support, not only in scope of practice but improved training and education, the ability of EMR's and EMT Basics to place SGA's. - Robert Barrix
There are many states that allow it, so expanding the scope is not a big change in much of the country. To me can have a more effective SGA seal for extraction/transport than you can for BVM. Also allows for one less person to focus on the airway (1 for BVM + 1 for bagging versus 1 for bagging with SGA). EtCO2 waveform recognition (not necessarily interpretation) must be part of it in order to verify appropriate placement. Should not lose BVM positioning and seal as a fundamental skill in EMS, though. - Joshua Stilley
There is some evidence for these assertions. In a simulation study of inexperienced providers (senior medical students and first year emergency medicine residents), inexperienced providers had more difficulty administering adequate tidal volumes with bag mask ventilation versus a laryngeal tube that they placed themselves. [3] In an Austrian study of EMTs (who have ~ 260 hrs of training), successful ventilation by laryngeal tube versus bag valve mask in out-of-hospital cardiac arrest was much higher in the SGA group (92%) versus the BVM group (35%). [4]. In a subsequent randomized study of 78 patients with OHCA, efficient ventilation by EMTs was also higher (though not significantly) with SGA (71.4%) compared with BVM (58.5%). [5] These studies defined “success” as the presence of adequate chest rise as assessed by a responding emergency physician - not End-tidal CO2 . Capnography use may further demonstrate unrecognized ventilation failure with BVM:
Confirmation of airway
One additional theme of the commentary is the importance of confirmation of effective ventilation with the use of capnography. Dr. Vithalani published an important article that demonstrated that unrecognized misplacement was a significant issue with SGAs as well, and that end-tidal capnography had a key role to play in monitoring for misplacement and ventilation failure:
Yes - but only if EtCO2 also included and crews adequately equipped. Rate of unrecognized misplacement may be as high as 14% - https://pubmed.ncbi.nlm.nih.gov/28750882/ - Veer Vithalani
His comments regarding the necessity of EtCO2 use were echoed by many others on the thread:
If not paramedic on-scene, we require EMT to use calorimetric ETCO2, but ALS required to follow up confirmation with quantitative/waveform capnography. -Ryan Jacobsen
Also, in Ohio, the use of waveform capnography is mandatory when for any invasive airway device, including supraglottic airway devices, are utilized. - Carol Cunningham
Tennessee utilizes this, ETCO2 is encouraged but only required at the ALS and CC levels, not at the BLS level. - Tyger Marie
Yes, as long as have EtCO2 and training. The use of EtCO2 should also be with BVM - Benjamin Abo
Michigan allows EMTs and EMR to place i-gel supraglottic airways. EMTs can also do King and Combitube but most are adopting i-gel. The decision is based on the agency and oversite organization (Medical Control Authority) choice. Use is not mandatory but is in the state protocols with local options for adoption. Our EMTs and EMRs typically use color change CO2 detection instead of waveform capnography. Agencies that use supraglottic airways must have CO2 detection or waveform capnography. - Robert Domeier
In review of state scope of practice, states that allowed for SGA use at the EMT level also allowed for capnography use by EMTs [Figure 1].
Training
One commenter, EMT GOOSE, simply wrote “Why on earth WOULDN'T you let an EMT place an SGA?”.
This is well addressed, I think, by the following anonymous comment:
“You're asking the wrong question. The better question is "Should EMT education prepare EMTs to place SGAs?" People are pushing to expand the EMT scope to include more advanced skills, but skills are the easy part. You could teach a monkey to jam a plastic tube into a hole and check for yellow squiggles on the screen.
Skills should be the result of education; they should not be the goal. Technicians learn skills: a cursory overview of who, what, when, where, why, and how to place an SGA can be taught in an afternoon. A clinician, however, is taught the underlying pathophysiology to such a degree that they can recognize the need for an advanced airway before ever learning the skill. If done right, a clinician could intuit at least the general operation of the SGA without being taught, based solely on their understanding of the concepts underlying the device.
Technicians get paid $12 an hour. Clinicians get a sustainable career.
As the saying goes, “Everybody wants to be a bodybuilder, but nobody wants to lift no heavy-*** weights.” “
This thought process was echoed by several others:
At some point we do need to differentiate levels of education and scope. The EMT scope can not continue to grow without addressing the actual content and time requirements of education to be eligible for testing at that level. If we continue to water downtime education and give out protocols and skills without education about physiology, pharmacology and disease we are not advancing the profession of EMS with clinicians but rather propagating technicians. - Herbert Schiffer
There was talk about in this protocol roll out, however the Medical Directors Practice Board who write our protocols added CPAP and albuterol to the EMT scope of practice. They decided that the BIAD would be too much to change and educate. In the interim we’re talking about a pilot project to trial Kings for EMT. - Stephen Smith
The skill itself is easy but recognizing where the airway went requires more training, education and experience. I agree with comments above about the importance of marrying airway management to EtCO2 monitoring. My system in Maryland sends two paramedics to every arrest so "shedding the airway load" isn't so much of a concern. I think the additional training (initial and on-going) and equipment costs would argue against us expanding the number of clinicians who can perform this skill. However, I could see in smaller systems, where the Medical Director and training staffs have a much tighter span of control, where this could be of use. - Alan Butsch
Yes, but only with commensurate increase in training time. As we keep increasing the scope and new skills, we spend less time on the basics to fit it into an already tight schedule. - Jason
We continue to add "procedures" to the EMT scope of practice, without increasing the underlying academic base. If we want to adopt the Canada "Primary Care Paramedic" model, let's increase the educational standards accordingly. To much "do" and not enough "know and understand."- Skip Kirkwood
Indeed this mirrors the reasoning cited in the National Scope of Practice model regarding additional skills in general:
“Some States permit licensed EMS personnel to perform skills and roles beyond the minimum skill set as they gain knowledge, additional education, experience, and (possibly) additional certification (See also Section III Specialty Care Delivered by Licensed EMS Personnel.) Care must be taken to consider the level of cognition and critical thinking necessary to perform a skill safely. For instance, some skills may be simple to perform, but require considerable clinical judgment to know when they should, and should not, be performed.”
The National Scope of Practice Model addresses minimum scope of practice. The average EMT-B program in the United States encompasses somewhere between 120-150 hours of education. Without increasing total time, everything added is a tradeoff; to add additional content, we can remove something, add flexibility at the agency level or collectively decide that the development and maturation of clinicians is truly the goal at all practice levels, which may not be achievable through this set limit of hours.
Summary
While SGA placement and capnography are not at the national EMT scope of practice, the majority of states have allowed this as an EMT skill either at the state scope of practice or by agency-sponsorship and training. There is evidence that from a skill-performance perspective, placement success is high and indeed, may be an easier psychomotor skill for inexperienced providers than effective bag valve mask ventilation (which clearly still remains critical). It is essential that SGA placement and capnography come together, as SGAs still can have placement failure. From the perspective of management of cardiac arrest, the indications are straightforward and may allow ALS clinicians to offload airway management and focus on the resuscitation overall. However, when considering adding a skill to the scope of practice, we must consider that this requires adding education to an already time-strapped curriculum, which should cover not only how to perform the skill, but when it should (or should not) be performed and how to monitor its effectiveness.
Discussion Forum Summary by EMS MEd Editor, Maia Dorsett, MD PhD FAEMS FACEP, @maiadorsett
References:
1. Bledsoe, B. E., Slattery, D. E., Lauver, R., Forred, W., Johnson, L., & Rigo, G. (2011). Can emergency medical services personnel effectively place and use the Supraglottic Airway Laryngopharyngeal Tube (SALT) airway?. Prehospital Emergency Care, 15(3), 359-365.
2. Gahan, K., Studnek, J. R., & Vandeventer, S. (2011). King LT-D use by urban basic life support first responders as the primary airway device for out-of-hospital cardiac arrest. Resuscitation, 82(12), 1525-1528.
3. Hart, D., Driver, B., Kartha, G., Reardon, R., & Miner, J. (2020). Efficacy of Laryngeal Tube versus Bag Mask Ventilation by Inexperienced Providers. Western Journal of Emergency Medicine, 21(3), 688.
4. Roth, D., Hafner, C., Aufmesser, W., Hudabiunigg, K., Wutti, C., Herkner, H., & Schreiber, W. (2015). Safety and feasibility of the laryngeal tube when used by EMTs during out-of-hospital cardiac arrest. The American journal of emergency medicine, 33(8), 1050-1055.
5. Fiala, A., Lederer, W., Neumayr, A., Egger, T., Neururer, S., Toferer, E., ... & Paal, P. (2017). EMT-led laryngeal tube vs. face-mask ventilation during cardiopulmonary resuscitation-a multicenter prospective randomized trial. Scandinavian journal of trauma, resuscitation and emergency medicine, 25(1), 1-7.